"Anti-cancer medicine, whether it can specifically attack cancer cells or not, needs to cut off molecular interactions between cancer cells and their environment, called tumor microenvironment, which help the cancer cells grow. Through blocking these interactions, we can reduce the cancer cells’ resistance against anti-cancer medicine, therefore preventing the tumor from spreading or relapsing."
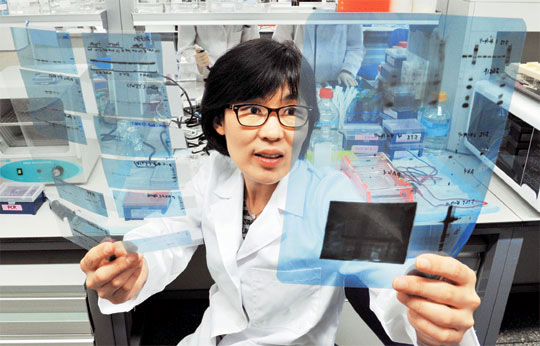
Professor LEE Ho-Young, from Seoul National University Department of Manufacturing Pharmacy stressed the importance of such methods in future anti-cancer medicine research. Professor Lee, who is a renowned specialist in anti-cancer research, said"Once cancer breaks out, preventing its relapse after first removing the tumor through surgery or chemotherapy is most important." The main goal of her research is to"discover the mechanism for how tumor microenvironment can induce the cancer cells to relapse." Professor Lee also added that"Finding methods to cure cancer that have spread to other organs is another important subject for me."
Professsor Lee, who received her Ph.D. from Ewha Womans University in 1992, finished her post-doctoral program in 1995 at the University of Texas. She received 6 months of research funding from the National Institutes of Health (NIH) three times while she was an assistant professor and received tenure from the University of Texas MD Anderson Cancer Center in 2009. The MD Anderson Cancer Center is a world-class institution in cancer research, where leaders of major companies including LEE Kun-hee are treated. Professor Lee worked 365 days a year, concentrating on her research. SNU appreciated her experience and efforts and offered Professor Lee a position. She accepted SNU’s offer and returned to Korea in March, 2011 to expand her research to studying the relations of cancer to other diseases. She majored in ‘translational research’, a study that connects anti-cancer research with effective clinical tests, and her experience in the field will help bring Korea’s anti-cancer research to a higher level.
Anticancer medicine is artificially synthesized or purified from natural materials and given to patients with various types of cancer. The medicine includes substances that can block enzymes synthesizing DNA, or molecules that act as pseudo-DNA which can interfere in DNA synthesis.
When DNA synthesis is blocked, cancer cells cannot replicate thereby stopping the growth of the tumor. However, since normal cells also need DNA to replicate, most anti-cancer medicine kills normal cells as well as cancer cells. This causes a lot of pain and has side effects such as vomiting. In order to prevent these problems, target anticancer medicine has been developed. Target anticancer medicine can kill the cancer cells specifically, by making antibodies that can only stick to the surface of cancer cells. These antibodies mark the cancer cells as targets for certain enzymes that can kill the targeted cancer cells. Although chemotherapy together with target anticancer medicine has decreased the side effects of previous anticancer treatment, preventing relapse or the spread of cancer cells still remains a problem for anticancer medicine research.
Professor Lee gave an interview introducing her research and her goals.
- You majored in translational research. What exactly is ‘translational research’?
‘Fundamental research’ refers to the process of making an hypothesis, then proving the hypothesis by experimenting with small organisms like bacteria and complex animal models such as dogs and cats. Medical doctors observe a patient’s physiological response for their research, a method which is called ‘clinical research’. There is a gap between fundamental research and clinical research, so translational research acts as a bridge between these two fields. Current translational research involves many projects where researching professors, doctors, pathologists, pharmaceutical chemists and statisticians have to work together as a team. I used to do translational research on lung cancer and head and neck cancer, which focuses on discovering which chemical in cigarettes induces lung cancer.
-How can anticancer medicine cure cancer?
There are many kinds of chemotherapy, each using different drugs such as alkylating reagents, plant alkaloids, metabolic antagonists, antioxidants and antibiotics. These drugs are artificially synthesized in laboratories or extracted from plants.
Anticancer medicine is simply based on the idea that since tumor cells replicate at an abnormally fast rate, more tumor cells can be killed compared to normal cells when replication is blocked. Therefore, the key to developing effective anticancer reagents is finding a way to block DNA synthesis. By inserting pseudo-DNA inside cancer cells or interfering with the reaction of polymerase, an enzyme that synthesizes DNA inside the cells, anticancer medicine can stop cell replication and kill cancer cells. Target anticancer medicine has been developed to maximize this process by selectively killing tumor cells.
- How do target anticancer drugs function?
There are many kinds of protein on the surfaces of tumor cells. Some of these surface proteins which are expressed at a higher level in tumor cells are called ‘receptors’. There are many growth factors - proteins that enable cells to grow - outside the cancer cell. The cancer cell can either produce its own growth factors, or get them from different parts of the body via blood circulation. The tumor microenvironment enables the growth factors to function properly. Then the growth factors bind to the receptors and start a molecular signal for cancer cell growth. This is the mechanism for tumor formation.
Target anticancer medicine can produce antibodies that can bind to the receptors. Growth factors cannot bind to the receptors that are bound to the antibodies, so the signal for cancer cell growth is cut off and further tumor formation is blocked.
Such antibodies that bind to receptors are called ‘biomarkers’. Since many different receptors are involved, doctors use ‘combination therapy’, through which a combination of several target anticancer drugs is used. Many different surface proteins of the cancer cells have to be blocked simultaneously; therefore many kinds of anticancer medicine and target anticancer medicine are combined for use in therapy.
- What are the limitations of using target anticancer medicine?
Cancer is a systematic disease, meaning the causes and effects of the disease are complex. Target anticancer medicine focuses on disrupting the interactions between the tumor cells and the tumor microenvironment that helps cell growth. However, cancer cells in the middle of their development can be modified during chemotherapy in a way that they can resist target anticancer drugs. These modified tumor cells remain and cause the cancer to relapse or spread to other organs. Our goal is to find an effective way to prevent cancer from relapsing or metastasizing. In order to do so, we need to develop ways to block the interaction of tumor cells and the tumor microenvironment.
- Treating stage 4 cancer still remains a problem in medical science. Can stage 4 cancer and its relapse or metastasis be cured using anticancer drugs?
Complete cure is not possible yet. Current chemotherapy only prolongs the patients’ life by preventing further growth of the tumor. Chemotherapy stops the tumor from growing, but the cancer cells are still there and they remain in the body by using different mechanisms from the original cancer cells. Therefore, it is important to prevent the cancer cells from spreading or relapsing by reducing stress. Maintaining a balanced lifestyle by meditating and eating regular, healthy meals can help. If you give stress to an animal by locking it up in a tightly enclosed space or taking its food away while it is eating, you can see that the animal is more likely to develop cancer cells that spread faster and easily metastasize.
- Why did you start your research on anticancer reagents and what made you decide to return to Korea?
I decided to have a career in research on treating cancer after my father died of liver cancer. In America, my research was used directly to treat patients, which gave me a huge sense of responsibility and motivated me to work harder. Although the MD Anderson Cancer Center has one of the best research infrastructures in cancer research and I was well-respected, my research was only confined to my major, lung cancer and head and neck cancer. Since cancer has many correlations with other diseases, I wanted to conduct research on other diverse areas such as gastric cancer, liver cancer and pancreatic cancer. My son, who lived with me in America, entered university which made me think more about returning to my family in Korea. Also, I was envious of Korean professors because they can educate and raise their own students. Currently I am continuing research on gene expression of metastasized cancer cells and doing a 5-year research project on ‘mechanisms and methodology for constraining lung carcinogenesis.’ I am also doing a co-project with the MD Anderson Center.
Professor Lee showed great enthusiasm for educating Korean students and researchers. She hopes to hand down her 16 years of experience, research methods and views to young Korean scientists. “Having research experience only in Korea is entirely different from doing research with an international perspective,” Professor Lee explains. She strongly emphasized that she “will try to do her best in both her research and teaching students.”
Written by JANG Eunju, SNU English Editor, ejjang1025@snu.ac.kr ?
Reviewed by Eli Park Sorensen, SNU Professor of Liberal Studies, eps7257@snu.ac.kr
Proofread by Brett Johnson, SNU English Editor, morningcalm2@gmail.com

